A 37 yr old male with burning sensation
A 37 yr old male presented with chief complaints of
burning sensation of both hands since 20days
lower limb pain since 20days
b/l knee pain since 20 days
HOPI
Pt was apparently asymptomatic 20 days ago then he developed burning sensation of both hands since 20 days more over nail beds , pain present over nail bed and has difficulty in performing daily activities. More insidious gradually progressive.No relieving factors.
H/o lower limb pain since 20 days which was insidious in onset gradually progressive aggravated on walking relieved on sitting
No sob, palpitations,orthopnea ,fever, pain abdomen,burning micturition
H/o chronic alcoholism since 20 years and consumes around 350-450ml daily ,last consumption of alcohol -yesterday 7pm 180ml H/o tobacco chewing since 20years
H/o pedal edema 1year back was admitted at local hospital and treated conservatively
PAST HISTORY
N/k/c/o DM, CVA, TB, EPILEPSY, HTN
DAILY ROUTINE
He daily wakes at 5 Am and takes bath and fresh up drinks tea at 7am and then he takes his breakfast (RICE with vegetable curry )at 8am and takes his lunch at 1 pm which consisting of a vegetable curry and rice and after his lich he chit chat with his neighbors and lie down for some time and after that he watch TV and then eats his dinner at 8pm and goes to sleep at 9pm.
PERSONAL HISTORY
Diet mixed
Appetite normal
Bowel and bladder -regular
Chronic alcoholic since 20 years
Tobacco chewing since 20years
GENERAL PHYSICAL EXAMINATION
On examination, patient is conscious, coherent, cooperative
patient is moderately built and moderately nourished
No pallor,icterus, cyanosis, clubbing, lymphadenopathy, edema
VITALS
temp afebrile
Bp 110/70mmhg
Pr 96bpm
Rr 18c/m
SYSTEMIC EXAMINATION:
Abdominal examination:
Inspection
Umbilicus inverted , No abdominal distention,no visible pulsations,scars and swelling.
Palpation
Soft, non tender, no organo megaly.
Auscultation
Bowel sounds Heard
Cardio vascular examination:
No visible pulsations, scars, engorged veins. No rise in jvp
Apex beat is felt at 5 Intercoastal space medial to mid clavicular line.
S1 S2 heard . No murmurs.
Respiratory system :
Shape of chest is elliptical, b/l symmetrical.
Trachea is central. Expansion of chest is symmetrical
Bilateral Airway Entry - positive
Normal vesicular breath sounds
CNS examination:
No neurological deficit found.
HMF Intact
Tone UL N N
LL N N
Power UL 4/5 4/5
LL 4/5 4/5
B +1 +1
T +1 +1
S. +1. +1
K. +1. +1
A. +1. +1
P. +1. +1
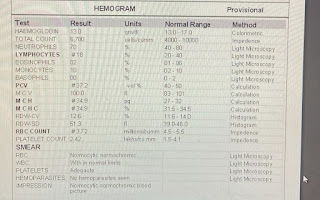
INVESTIGATIONS
Psychiatric referral in view of alcohol addiction and tobacco chewing
Impression: Alcohol dependence syndrome Advice given: Tab Lorazepam 2mg
X -X - 2
Psychiatric follow up done
Advice: Tab Lorazepam 2mg
1-1-2
Tab Baclofen XL 20mg
1-X-1
Continue thiamine supplementation
Psychiatric follow up done
Advice: Tab Lorazepam 2mg
1-1-2
Tab Baclofen XL 20mg
1-X-1
Continue thiamine supplementation
Monitor vitals 2nd hourly
PROVISIONAL DIAGNOSIS
Peripheral Neuropathy secondary to alcohol (Dry ber beri)
Alcohol withdrawal state
TREATMENT
1)Iv fluids NS @ 75ml/hr.
2)Inj THIAMINE 200mg in 100ml NS /IV/ TID
3)OPTINEURON lamp in 100 ml NS /IV / OD.
4)T. PREGABALIN -M PO/HS
X-X-8pm
5)Tab Lorazepam 2mg
1-1-2
6)Tab Baclofen XL 20mg
1-X-1
::SUMMARY::
DIAGNOSIS
Peripheral Neuropathy secondary to alcohol (Dry ber beri)
Alcohol withdrawal state
burning sensation of both hands since 20days
lower limb pain since 20days
b/l knee pain since 20 days
On clinical examination he had
VITALS:
temp afebrile
Bp 110/70mmhg
Pr 96bpm
Rr 18c/m
GENERAL EXAMINATION:
No pallor,icterus, cyanosis, clubbing, lymphadenopathy, edema
SYSTEMIC EXAMINATION:
Abdominal examination:
Inspection
Umbilicus inverted , No abdominal distention,no visible pulsations,scars and swelling.
Palpation
Soft, non tender, no organo megaly.
Auscultation
Bowel sounds Heard
Cardio vascular examination:
No visible pulsations, scars, engorged veins. No rise in jvp
Apex beat is felt at 5 Intercoastal space medial to mid clavicular line.
S1 S2 heard . No murmurs.
Respiratory system :
Shape of chest is elliptical, b/l symmetrical.
Trachea is central. Expansion of chest is symmetrical
Bilateral Airway Entry - positive
Normal vesicular breath sounds
CNS examination:
No neurological deficit found.
HMF Intact
Tone UL N N
LL N N
Power UL 4/5 4/5
LL 4/5 4/5
B +1 +1
T +1 +1
S. +1. +1
K. +1. +1
A. +1. +1
P. +1. +1
COURSE IN THE HOSPITAL
PATIENT WAS ADMITTED IN VIEW OF BURNING SENSATION OF BOTH HANDS SINCE 20 DAYS LOWER LIMB PAIN SINCE 20 DAYS AND BILATERAL KNEE PAIN SINCE 20 DAYS AND WAS INVESTIGATED FURTHER AND FOUND TO HAVE DERANGED FT AND TREATED CONSERVATIVELY PSYCHIATRY REFERRAL IN VIEW OF ALCOHOL ADDICTION AND TOBACCO CHEWING.
6/5/23
PSYCHIATRIC REFERRAL IN VIEW OF ALCOHOL ADDICTION AND TOBACCO
CHEWING
IMP: ALCOHOL DEPENDENCE SYNDROME TOBACCO HARMFUL USE CURRENTLY
ABSTINENT
ADVICE TAB LORAZEPAM 2MG X-X-2
7/5/23:
PSYCHIATRY FOLLOWUP DONE AND ADVICED TAB LORAZEPAM 2MG 1-1-2
TAB BACLOFEN 20MG 1-X-1
7/523
PSYCHIATRY FOLLOWUP DONE AND ADVICE TAB LORAZEPAM 2MG 1-1-2
TAB BACLOFEN 20MG 1-X-1
8/5/23
PSYCHIATRY FOLLOWUP DONE AND ADVICED TAB LORAZEPAM 2MG 1-1-2
TAB BACLOFEN 20MG 1-X-1
CONTINUE THIAMINE SUPPLEMENTATION
9/5/23:
PSYCHIATRY FOLLOWUP DONE AND ADVICED TABILORAZEPAM 2MG 1-X-2
TAB.BACLOFEN 20MG 1-X-1
CONTINUE THIAMINE SUPPLEMENTATION
PATIENT WAS COUNCELLED FOR ADMISSION TO DE ADDICTION CENTRE BUT HE REFUSED FOR THE SAME PATIENT WAS DISCHARGED IN STABLE CONDITION
Advice at Discharge
T THIAMINE 100MG PO BD
T.PAN 40MG PO OD
T.PREGABALIN M POHS
T LORAZEPAM 2MG 0-0-1
T BACLOFEN XL 20MG 1-X-1





























Comments
Post a Comment